Urban Poor and their Health Challenges
Once upon a time, in a sprawling metropolis – a liftman (resident of a slum) had severe cough from weeks and went on taking medicines from local doctors or quacks. Scared of losing his job, he didn’t tell about it to anyone. As he was on medication under local doctor without proper diagnosis, his undiagnosed TB turned into MDR (Multi-drug resistant) TB. Later, this Tuberculosis spread among the people who used to use the lift that he operated. One undiagnosed case led to many others. This is not a tale out of any story book; but the reality that exists across urban areas in our country.
Let’s start with understanding what an urban area is. An urban area can be largely defined as a densely populated area with built-up settlements of bricks-and-mortar continuity. These areas provide great opportunities for individuals and families to prosper and can provide a healthy living environment through enhanced access to services, culture and recreation. The recent times have seen that the growth of urban areas in low-income countries has been four times faster than the growth in high-income countries. The rapid migration from rural areas aided with the natural population growth is putting further pressure on limited resources in cities, especially in low-income countries. According to WHO (World Health Organization), by 2030, 6 in 10 people will be living in the towns and cities. In India, percent of slum dwellers have decreased from 24 (in 2001) to 22 percent (in 2011); on the other hand absolute numbers increased from 52 million to 65 million.
As mentioned above most of the migration takes place in search of better opportunities and services. Not all of them are from economically sound and highly qualified background. They get engage into the low-income jobs and prefer living in the slums and squatter settlements. These settings tend to be unregulated precarious, overcrowded, and are often exposed to hazards, such riverbanks and water basin locations subject to flooding, or sites near industrial hazards. They rely on street food, processed and cheap food; leading to nutritional problems such as vitamins/mineral deficiencies, etc. Inadequate diet reduces their resistances to diseases.
Health is valued universally as an essential prerequisite for a fulfilling and productive life. In fact, “Good Health and well-being” is included as the third goal of Sustainable Development Goals (SDGs), making it a matter of priority. Within this, Urban Health is emerging as a new and dynamic field, which brings to the fore the complex manner in which many factors are interlinked with each other. In the Indian context, urban health infrastructures have been found to be inadequate to meet the need of the urban population, especially the poor. There are 1083 Urban Family Welfare Center (UFWCs), and 871 Health Posts (HPs) that cater to 377 million people living in urban. This means one UFWC/HP per 192,992 urban populations. Such a number is naturally a discouraging factor for the poor people to approach government facilities. This is the reason the population living in poverty, even in urban areas, ends up seeking treatment from local quacks at cheap prices, majorly to save their wage loss.
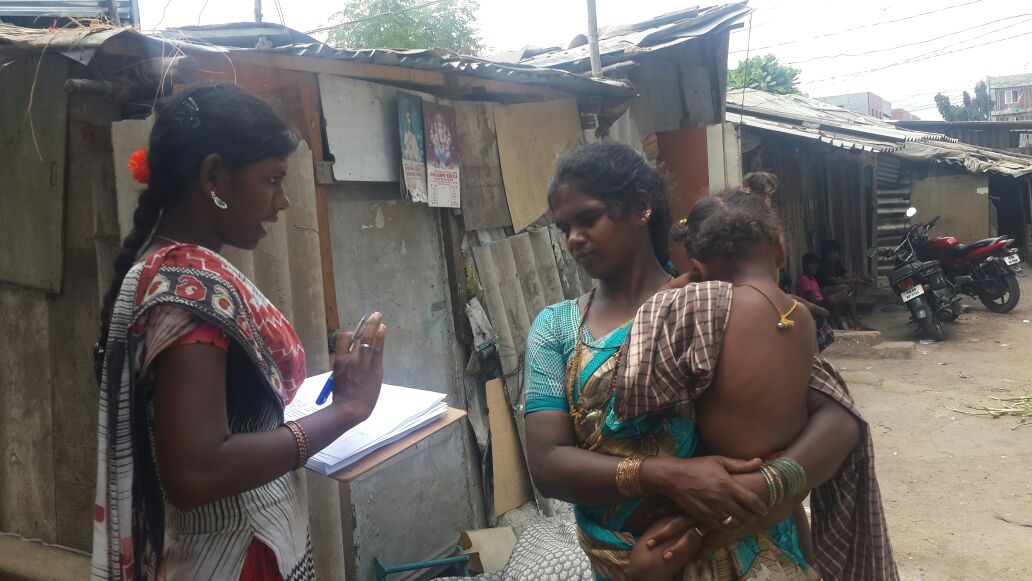
On one hand, the government has provided many policies for help of the needy (of which most people remain unaware), on the other hand the procedure is so time taking and complex, that it acts as a discouraging factor for even those who do have knowledge about the policy. While in the governmental setup, there is a lack of modern infrastructures for the proper diagnosis, it is easily available in the private sector but at a much higher cost. Added to these financial disparities, there are many factors which discourage poor from getting proper treatment, such as staff behavior, non-standardization of treatment and payment protocols and accessibility. The very low availability of urban health services for the urban poor and the non-functioning of those that are available indicate a serious lapse on the part of the government in urban health planning.
Faced with these issues, the populations living in poverty (which form the majority), end up opting for local doctors or quacks which further leads to the difficult health situations and spread of diseases. It is no wonder; this cycle repeats itself as reality for poor people across the urban areas in the cities.
